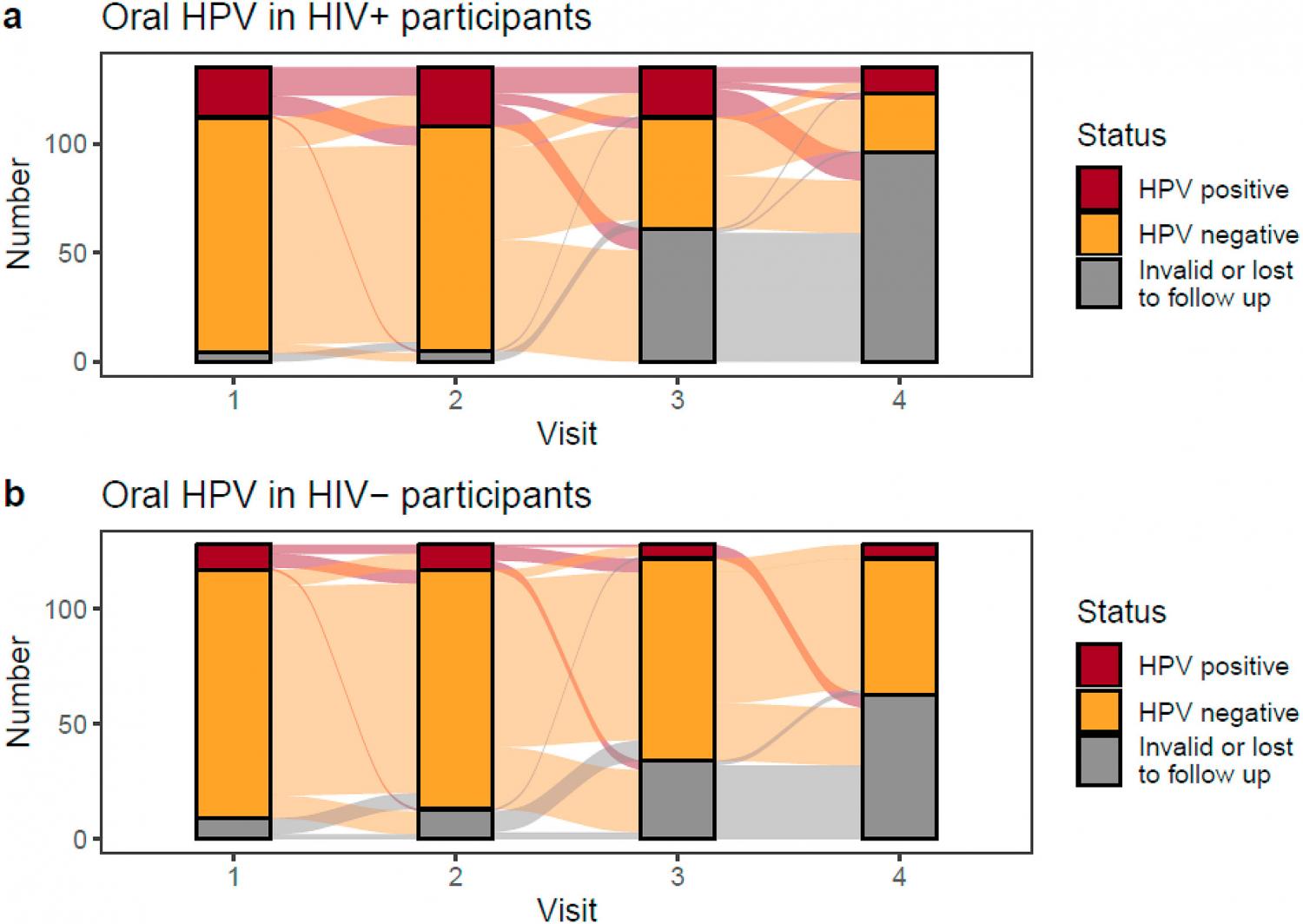
Background: HIV has been shown to increase the likelihood of oral HPV infection. In this study, we evaluated the risk of oral HPV in HIV infected patients compared with HIV-negative controls. Methods: 101 healthy adult volunteers (HIV-) and 245 adults living with HIV infection (HIV+) were recruited from 5 academic medical centers. Questionnaires and saliva samples were obtained every 3–8 months over a period of 2 years (2015–2017). DNA was isolated from the saliva samples and tested for 18 high- and low-risk genotypes. Results: Oral HPV was detected in 23% of HIV + vs. 10% of HIV- participants (p < 0.0001). Men had a higher oral HPV prevalence than women (27% vs. 15% HIV+, p = 0.03, 16% vs. 5% HIV-, p = 0.01). Risk factors among HIV + participants included more lifetime deep kissing and oral sex partners, and history of AIDS. Persistent oral HPV was detected in 23% of HIV + vs. 5% of HIV- participants (p < 0.001). Among 8 HIV + participants with CD4 counts <200 cell/μL none had cleared their HPV infection during the study. Conclusions: Risk of oral HPV infection and persistence was significantly higher in HIV + adults with a history of poorly controlled HIV, which may put them at increased risk of HPV-associated cancer.
