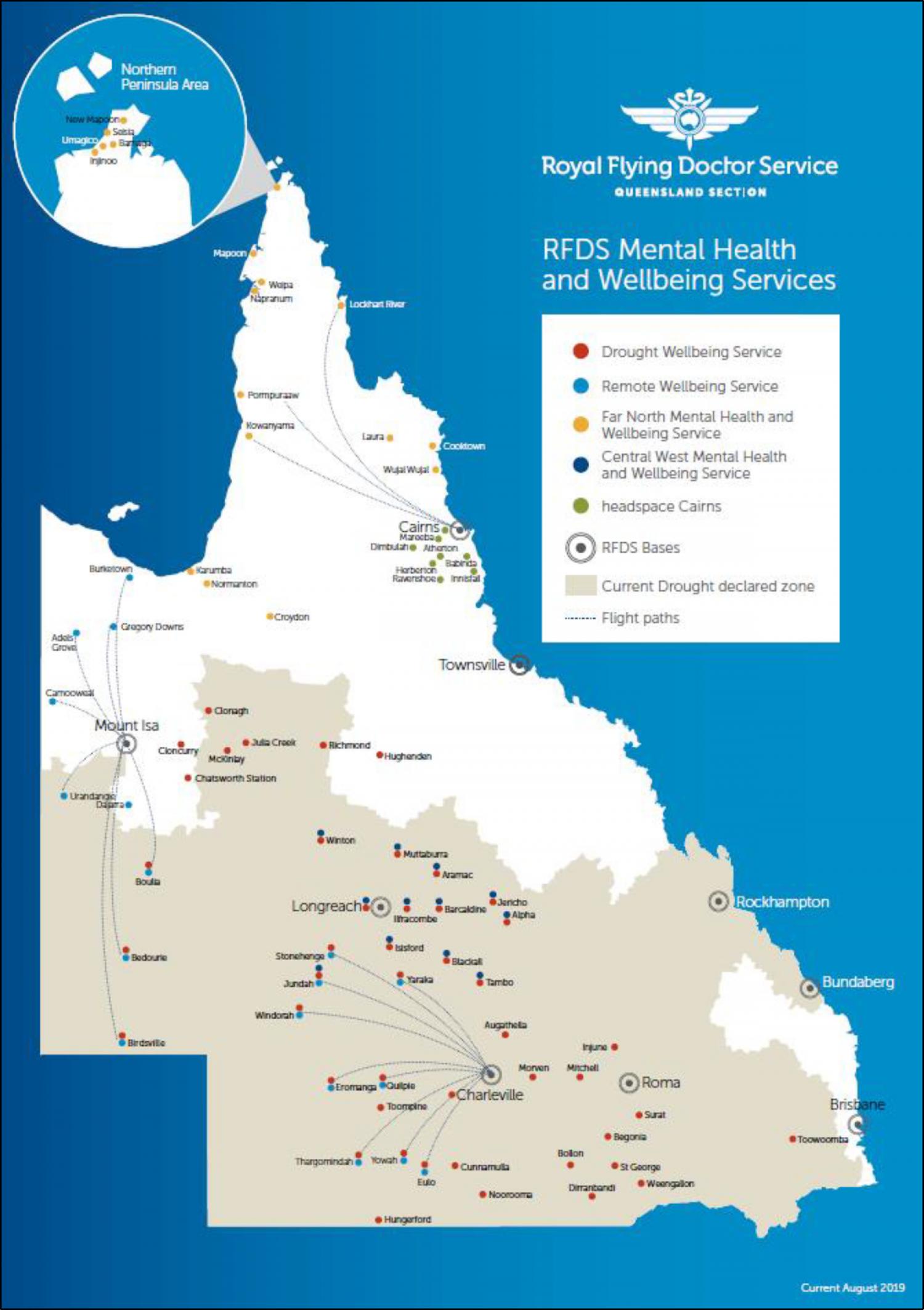
Background: Understanding cultural differences between geographical regions is essential in delivering culturally appropriate healthcare. We aimed to describe the characteristics and outcomes of diverse clients using the Far North Mental Health and Wellbeing Service (FNS) and the Central West Health and Wellbeing Service (CWS). Methods: We conducted a cohort study within Queensland, Australia, on all clients who received a mental health therapy session at either the FNS or the CWS. Patient data was prospective data collected form July 2019 to December 2020. Findings: There were1202 clients, with a median number of individual contacts per-client of 3.0 (IQR 2.0-6.0). There was 428 (35.6% 95% CI 32.90-38.39) males and 772 (64.2% 95% CI 61.44-66.94) females with a median age across the genders of 38.0 (IQR 28.0-51.0). There was 505 (42.0% 95% CI 39.20-44.86) identifying as Indigenous and 697 (58.0% 95% CI 55.14-60.80) as non-Indigenous Australians. The FNS had a significantly higher proportion of Indigenous clients (n=484; 54.8% 95% CI 51.46-58.13) as compared to the CWS (n=21; 6.6% 95% CI 4.12-9.89). Of the 1202 clients, 946 (78.7% 95% CI 76.28-80.99) had a socio-economic classification of ‘most disadvantaged’, consisting of 740 (83.8%) clients from the FNS and 206 (64.6%) clients from the CWS. The majority of presentations were for neurotic, stress-related and somatoform disorders (n=568; 47.3%), followed by mood affective disorders (n=310; 25.8%). The overall number of treatments strategies employed was 10798, equalling a median of 6.0 (IQR 4.0-9.0) strategies per-client, with the leading strategies being counselling/psychosocial (n=1394; 12.9%), reflective listening (n=1191; 11.0%), and strengths based reasoning (n=1116; 10.3%). There were 511 (42.5%) clients who completed the Kessler Psychological Distress Scale (K10/K5), with 493 (41.0%) clients not offered as deemed not culturally appropriate by the treating team. The mean initial K10/K5 score was 23.7 (SD 9.4) which significantly decreased (p<0.001) to 18.0 (SD 10.0) at final consultation. Interpretation: This study highlighted client socioeconomic differences between two geographically remote mental health services. It is essential that services are regionally co-designed to ensure cultural appropriateness. Funding: No funding to declare.
