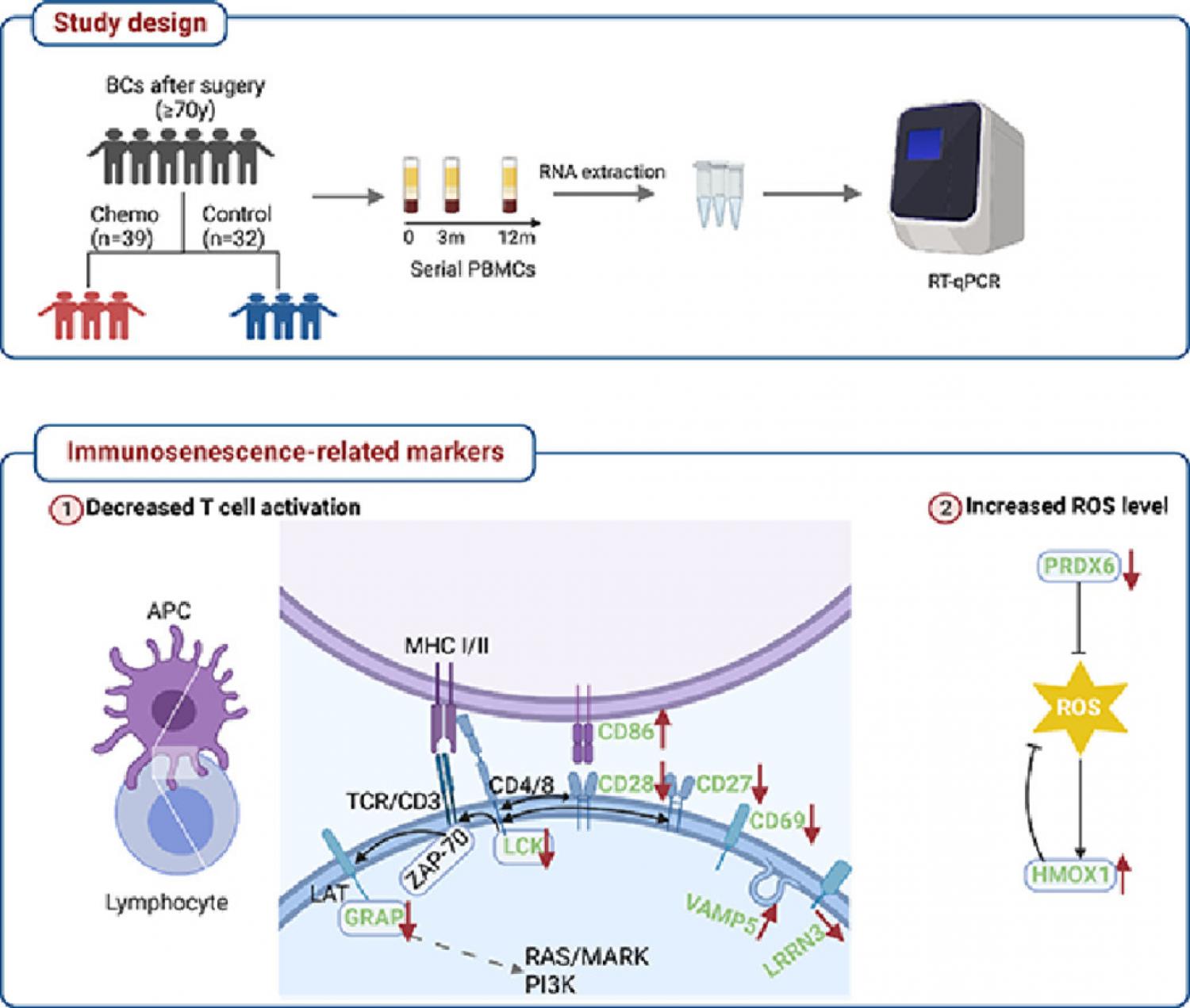
Background: The exact impact of chemotherapy on the immune system of older patients with breast cancer is not well known. A longitudinal study was performed investigating the evolution of the blood immune profile during and after chemotherapy in this population. Patients and Methods: The study included 39 patients receiving adjuvant chemotherapy (chemotherapy group, CTG) and 32 patients receiving only hormone therapy (control group, CG). A 10-gene panel associated with immunosenescence was measured in peripheral blood mononuclear cells (PBMC) before (T1), at 3 months (T2) and at 12 months (T3) after initiation of adjuvant therapy. Nutrition status was assessed by using a mini nutritional assessment scale. Linear mixed model analyses were performed for trajectory evolution, with or without adjusting for age, tumor stage, breast cancer phenotype, and/or corresponding baseline gene levels. Results: Six genes relating to T cell activation (CD28, CD27, CD86, LCK, GRAP, LRRN3), and two genes relating to oxidative stress (PRDX6, HMOX1) exhibited a significant group-by-time effect, even after adjusting covariates(p≤ 0.01). In CTG, the T cell activation genes substantially declined from T1 to T2 and bounced back to a level higher than baseline at T3 (p<0.03), which was not observed in CG (p>0.26). Patients with malnutrition detected at T1 experienced more pronounced perturbation regarding CD27, LCK, CD69, VAMP5, and LRRN3 (p<0.05). Conclusion: Chemotherapy leads to transient perturbation of immune-related gene expression and potentially stimulates immunity in the long term. Well-nourished patients experience less impact of chemotherapy on immune-related gene expression profiles.
