Elsevier, The Lancet Public Health, Volume 6, November 2021
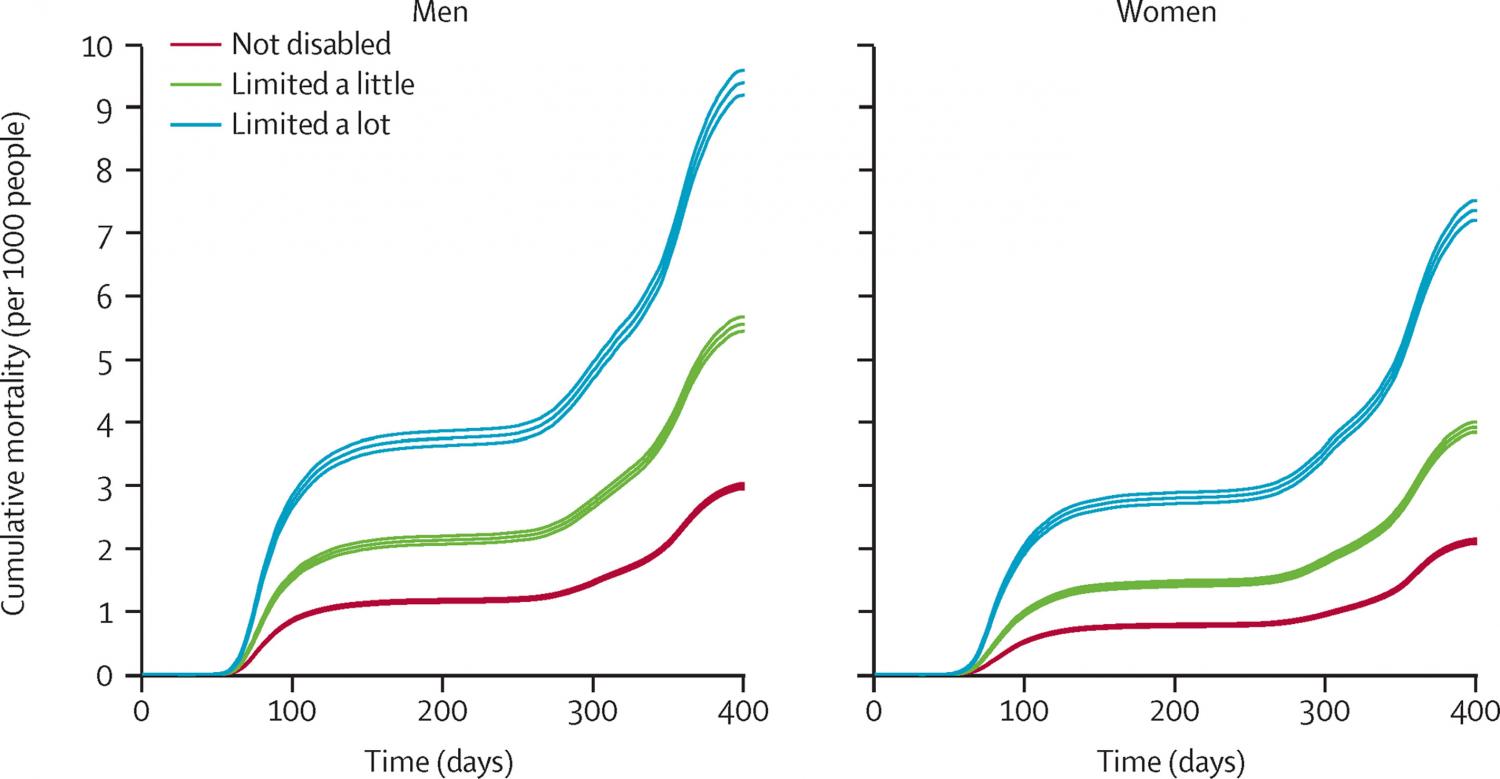
Background: People with learning disabilities are at substantially increased risk of COVID-19 mortality, but evidence on risks of COVID-19 mortality for disabled people more generally is limited. We aimed to use population-level data to estimate the association between self-reported disability and death involving COVID-19 during the first two waves of the COVID-19 pandemic in England. Methods: We conducted a retrospective, population-based cohort study of adults aged 30–100 years living in private households or communal establishments in England, using data from the Office for National Statistics Public Health Data Asset. Participants were present at the 2011 Census and alive on Jan 24, 2020. Participants reported being limited a lot in their daily activities, limited a little, or not limited at all, in response to a question from the 2011 Census. The outcome was death involving COVID-19, occurring between Jan 24, 2020, and Feb 28, 2021. We used Cox proportional hazards regression to calculate hazard ratios (HRs) for the association between disability and death involving COVID-19, sequentially adjusting for age, residence type (private household, care home, or other communal establishment), geographical characteristics (local authority district and population density), sociodemographic characteristics (ethnicity, highest qualification, Index of Multiple Deprivation decile, household characteristics [National Statistics Socio-economic Classification of the household reference person, tenure of household, household size, family status, household composition, and key worker in household], key worker type, individual and household exposure to disease, and individual and household proximity to others), and health status (pre-existing health conditions, body-mass index, and number of admissions to hospital and days spent in hospital over the previous 3 years). Findings: 29 293 845 adults were included in the study (13 806 623 [47%] men, 15 487 222 [53%] women), of whom 3 038 772 (10%) reported being limited a little and 2 011 576 (7%) reported being limited a lot. During follow-up, 105 213 people died from causes involving COVID-19 in England, 61 416 (58%) of whom were disabled. Age-adjusted analyses showed higher mortality involving COVID-19 among disabled people who were limited a lot (HR 3·05 [95% CI 2·98–3·11] for men; 3·48 [3·41–3·56] for women) and disabled people who were limited a little (HR 1·88 [1·84–1·92] for men; 2·03 [1·98–2·08] for women) than among non-disabled people. Adjustment for residence type, geography, sociodemographics, and health conditions reduced but did not eliminate the associations between disability and death involving COVID-19 (HR 1·35 [1·32–1·38] for men who were limited a lot; 1·21 [1·18–1·23] for men who were limited a little; 1·55 [1·51–1·59] for women who were limited a lot; and 1·28 [1·25–1·31] for women who were limited a little). Interpretation: Given the association between disability and mortality involving COVID-19, verification of these findings and consideration of recommendations for protective measures are now required. Funding: None.
