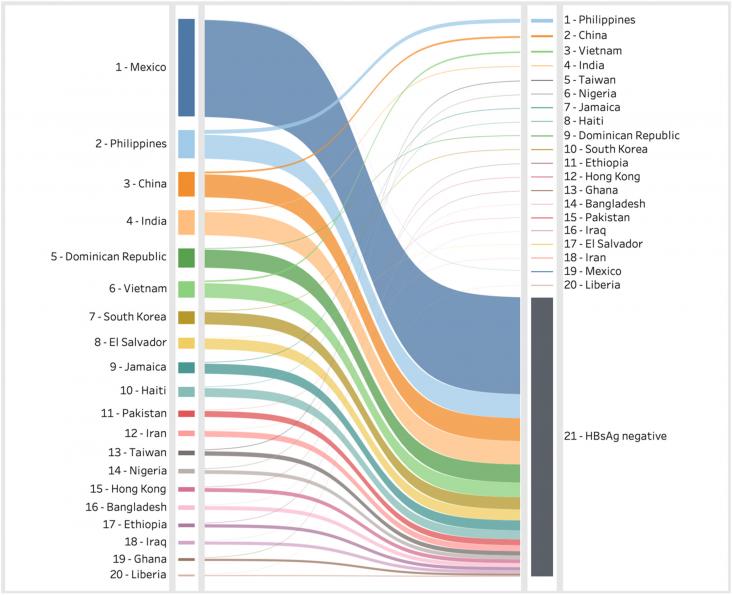
This Article supports SDG 3 by using modelling to estimate the impact of immigration on hepatitis B prevalence in the USA, in order to more accurately assess the hepatitis B burden, which might not be accurately measured by national serosurveys. The study found a significantly higher burden of hepatitis B (1.8 million cases), significantly higher than that found in national serosurveys.
This Article supports SDG 3 by assessing the incidence of HIV and HCV infection among people who inject drugs, a population at higher risk of these infections. In this systematic review, HCV estimates came from studies in 24 countries. Pooled HCV incidence was 12.1 per 100 person-years; data for both infections were scarce, suggesting increased efforts are needed to keep track of these infections in this population.
This Article supports SDG 3 by estimating the burden of low back pain, which continues to be the leading cause of disability worldwide. The study predicts that low back pain prevalence will continue to increase, from 619 million people in 2020 to 843 million in 2050. Two-fifths of the burden are due to modifiable risk factors, and a quarter of years lived with disability are attributable to occupational ergonomic factors.
This paper concludes that findings suggest that 1) long-term omega-3 fatty acid supplementation may reduce risk of Alzheimer’s disease (AD); 2) dietary omega-3 fatty acid intake, especially DHA, may lower risk of dementia or cognitive decline; and 3) peripheral biomarkers of omega-3 fatty acids may serve as predictors of cognitive decline. However, further investigation is needed to understand the gene–environment interactions involved in the intake of omega-3 fatty acids.
In this review, we discuss how cellular senescence contributes to brain aging and neurodegenerative diseases, and the relationship between protein aggregation and cellular senescence.
This study aimed to investigate the amelioration effects of preventive TEAS treatment (P-TEAS) on cognitive impairment and oxidative stress in AD model rats.
This article explores the potential of Traditional Chinese Medicine (TCM) as a treatment for Alzheimer's disease, highlighting the holistic approach of TCM and its promising results in improving cognitive function in Alzheimer's patients. It emphasizes the need for further rigorous clinical trials to validate these findings.