Hypertension, commonly known as high blood pressure, is a critical global health issue with a significant impact on several of the United Nations' Sustainable Development Goals (SDGs). This condition, characterized by persistently high pressure in the arteries, can lead to serious health problems, including heart disease, stroke, and kidney failure. The intersection of hypertension with the SDGs is multifaceted, demonstrating the interconnected nature of health and broader societal challenges.
The most direct link is with SDG 3, which focuses on Good Health and Well-being. This goal emphasizes the importance of ensuring healthy lives and promoting well-being at all ages. Hypertension is a major risk factor for cardiovascular diseases, the leading cause of death worldwide. Addressing hypertension is crucial for achieving SDG 3 targets, particularly those related to reducing non-communicable diseases and promoting mental health. This requires accessible and quality healthcare services for the detection, treatment, and control of hypertension, along with public health policies that prioritize cardiovascular health.
Hypertension also intersects with SDG 2, Zero Hunger, which aims to end hunger, achieve food security, improve nutrition, and promote sustainable agriculture. Diet plays a significant role in the prevention and management of hypertension. A balanced diet, low in salt and rich in fruits, vegetables, and whole grains, can help lower blood pressure. Therefore, efforts to provide access to nutritious food and promote healthy eating habits directly contribute to the management and prevention of hypertension.
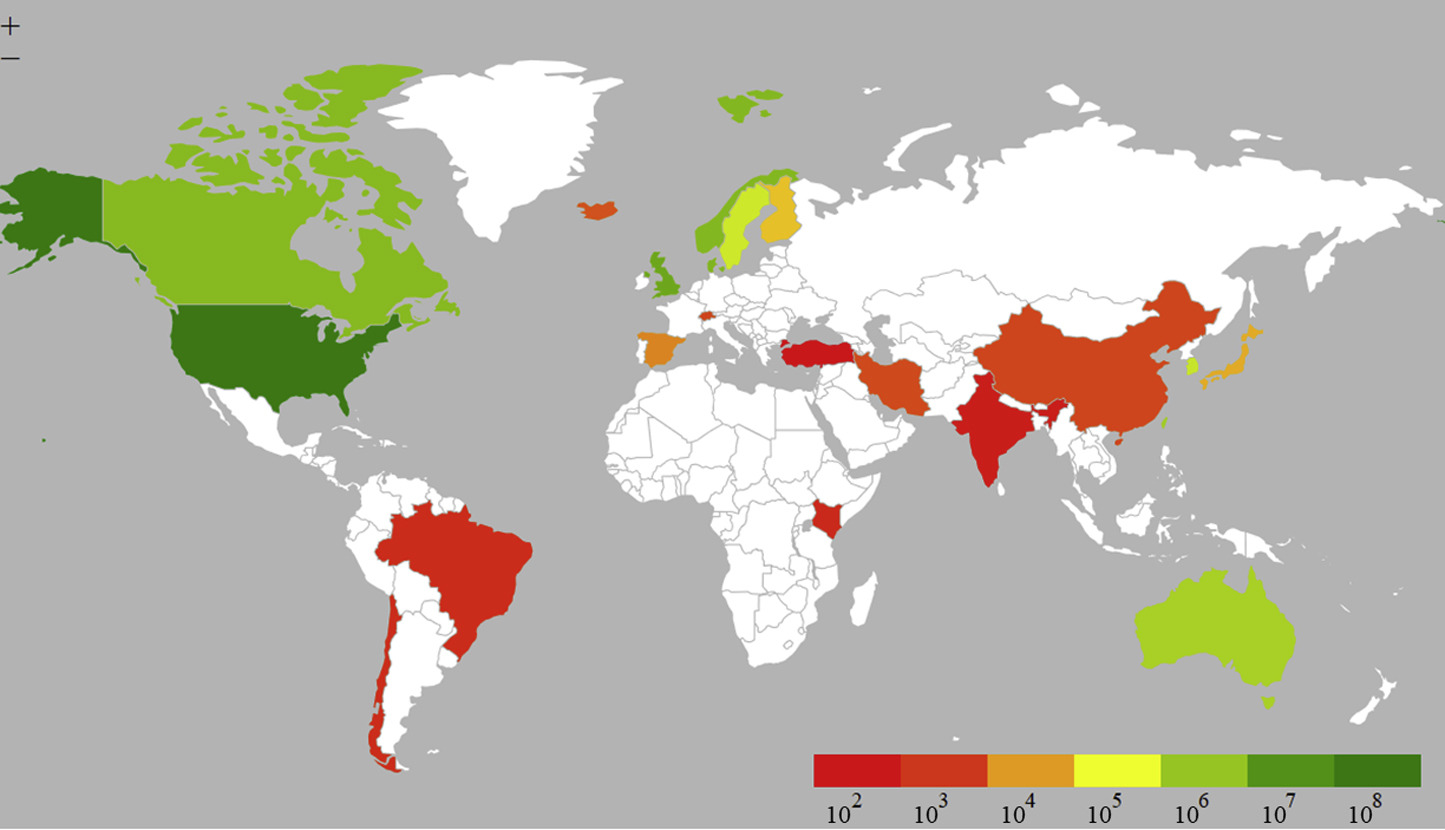
The condition has indirect implications for SDG 1, No Poverty, and SDG 10, Reduced Inequalities. Hypertension often disproportionately affects low- and middle-income populations. These groups are more likely to experience barriers to healthcare access, leading to delayed diagnosis and treatment. The economic burden of managing hypertension can exacerbate poverty, while the lack of resources in disadvantaged communities can limit access to preventive measures and treatment. This reflects and exacerbates existing socioeconomic inequalities, making it imperative to address hypertension as part of efforts to reduce poverty and inequality.
Furthermore, the awareness and prevention strategies necessary to combat hypertension tie into SDG 4, Quality Education. Educating the population about hypertension, including its risk factors, prevention, and management, is essential. Health literacy, part of broader educational goals, enables individuals to make informed decisions about their health and adopt healthier lifestyles. Efforts to incorporate health education into school curricula and community programs can significantly contribute to the prevention and control of hypertension.
Hypertension is not just a health issue but a multifaceted challenge that intersects with various SDGs. Addressing it requires a holistic approach that includes accessible healthcare, nutritional awareness, poverty alleviation, and educational initiatives. By tackling hypertension, we can make significant progress towards achieving several of the SDGs, demonstrating the interconnectedness of health and broader social and economic goals.
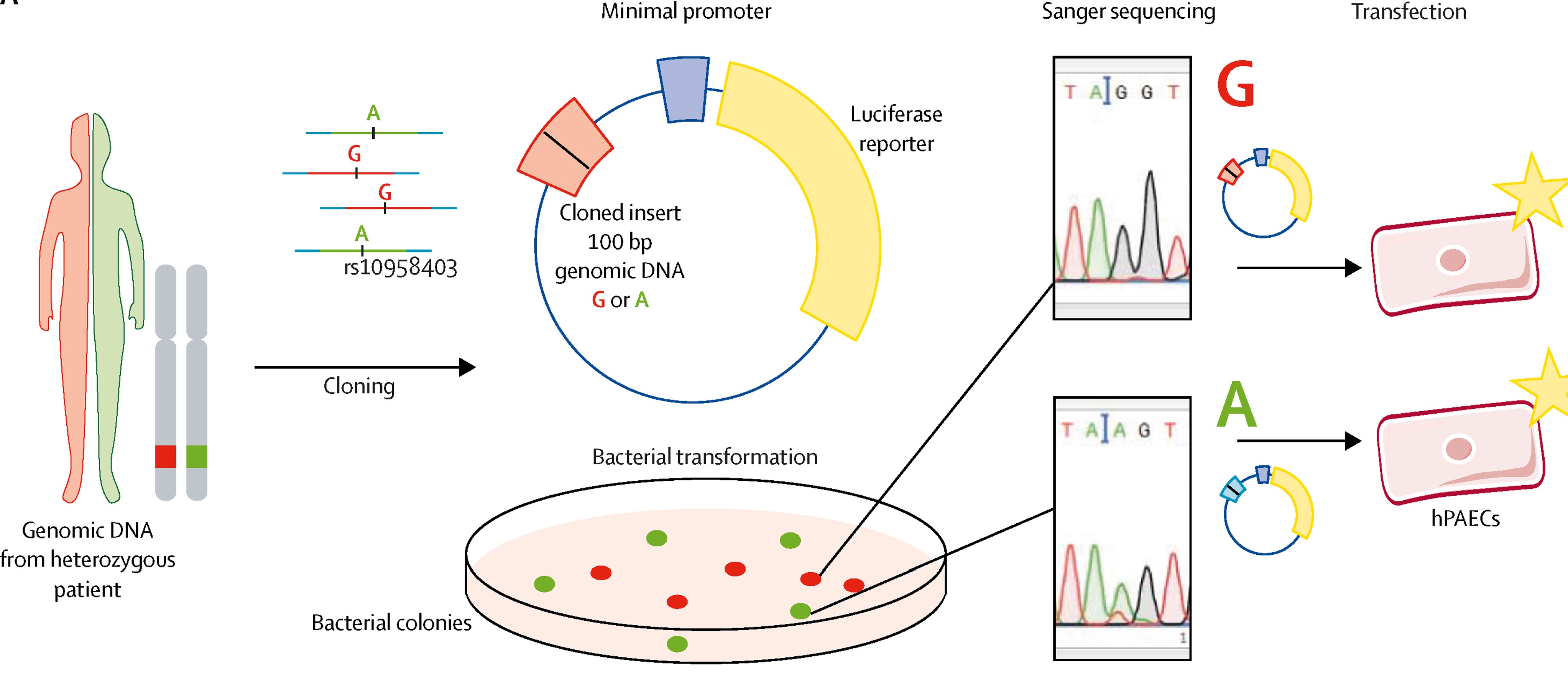
Pulmonary arterial hypertension (PAH) occurs in women more than men whereas survival in men is worse than in women. In recent years, much research has been carried out to understand these sex differences in PAH. This article discusses clinical and preclinical studies that have investigated the influences of sex, serotonin, obesity, estrogen, estrogen synthesis, and estrogen metabolism on bone morphogenetic protein receptor type II signaling, the pulmonary circulation and right ventricle in both heritable and idiopathic pulmonary hypertension.